Wisdom teeth, or third molars, often necessitate extraction due to their propensity to cause dental complications. These late-emerging teeth can become impacted, leading to overcrowding, misalignment, and even periodontal disease. Insufficient jaw space frequently traps these molars, contributing to infection and discomfort. Early radiographic evaluation and strategic intervention are paramount. Understanding the intricacies of their development and potential issues prompts further exploration into ideal management strategies for preserving oral health.
The Evolutionary Background of Wisdom Teeth
Wisdom teeth, also known as third molars, are vestigial structures that reflect the evolutionary history of the human dentition. These teeth once played a significant role in the diet of ancestral hominins, which included rough, fibrous plant material requiring substantial mastication. The evolutionary significance of wisdom teeth is rooted in their function as a dental adaptation to a diet that demanded extensive chewing. However, as human diets evolved and cooking methods softened food, the need for a third set of molars diminished. Consequently, the reduced jaw size in modern humans often lacks the space to accommodate these teeth, leading to potential complications. The evolutionary trajectory of dental adaptation underscores the redundant nature of wisdom teeth in contemporary human oral anatomy.
Understanding the Timing of Wisdom Teeth Emergence
The emergence of third molars, commonly referred to as wisdom teeth, typically occurs between the ages of 17 and 25, coinciding with late adolescent or early adult developmental milestones. This process is marked by specific clinical signs, such as gingival inflammation and swelling, which indicate the initiation of eruption. Understanding these chronological patterns and physiological indicators is essential for dental professionals in determining ideal intervention strategies.
Typical Age Range
Typically emerging between the ages of 17 and 25, third molars, commonly known as wisdom teeth, often coincide with the final stages of jaw development. This period marks a critical phase in dental development, as the jaws of young adults reach near-completion of growth. As these molars erupt, they may encounter spatial limitations within the oral cavity, potentially leading to impaction or misalignment. The timing of emergence aligns with the cessation of significant jaw growth, which provides minimal adaptability for accommodating these additional teeth. Consequently, dental professionals closely monitor this age range to assess potential complications. Early evaluation and intervention during this developmental window can preemptively address issues, optimizing oral health outcomes and reducing the risk of future dental complications.
Developmental Milestones
Emergence of third molars, or wisdom teeth, is an integral aspect of human dental development, occurring after the other permanent teeth have erupted. Typically, these third molars manifest between ages 17 and 25, marking a key developmental milestone in tooth development. During this period, the jaws have usually reached near-full maturity, which ideally accommodates the new molars. However, insufficient jaw space often complicates this process, potentially impacting oral health. The developmental trajectory of wisdom teeth is influenced by genetic and environmental factors, which dictate their alignment and emergence. Malocclusion, impaction, or partial eruption may arise when space is inadequate, necessitating clinical intervention. Understanding these developmental milestones is essential for dental professionals in optimizing patient oral health through timely assessment and potential removal.
Signs of Eruption
When do wisdom teeth typically begin to make their presence known? Wisdom teeth, or third molars, generally commence eruption between the ages of 17 and 25. The emergence is marked by discernible signs of eruption and various dental symptoms. Clinically, patients may report discomfort localized to the posterior mandibular or maxillary regions, which can manifest as pain, swelling, or tenderness. Radiographic evaluation often reveals the orientation and position of these molars, aiding in prognosis. Gingival irritation and pericoronitis are common, resulting from partial eruption, where the tooth breaks through the gingiva but fails to fully emerge. Dental practitioners must remain vigilant during routine examinations, as early detection of these symptoms facilitates timely intervention, potentially mitigating complications associated with impacted or malpositioned wisdom teeth.
Common Issues Associated With Wisdom Teeth
A multitude of complications can arise from the presence of wisdom teeth, clinically known as third molars. These teeth may remain impacted, failing to fully erupt into the oral cavity, which can lead to pericoronitis, an inflammatory condition often resulting in pain and swelling of the surrounding gum tissue. Additionally, the partial eruption of wisdom teeth can create an environment conducive to bacterial accumulation, complicating dental hygiene and increasing the risk of caries and periodontal disease. Moreover, the proximity of third molars to the mandibular nerve and maxillary sinus can pose significant challenges, potentially resulting in neuropathic pain or sinus complications. Radiographic evaluation and clinical assessment are essential for identifying these issues, guiding decisions on prophylactic extraction to mitigate potential oral health risks.
Overcrowding: When There’s Not Enough Space
Inadequate space within the dental arch often results in overcrowding, a common issue associated with the eruption of third molars. Space constraints can lead to misalignment of adjacent teeth, as the dental arches typically do not accommodate the additional molars. This overcrowding disrupts dental alignment, potentially causing malocclusion and increasing the risk of periodontal disease due to difficulty in maintaining oral hygiene. Orthodontic assessments frequently reveal that the presence of third molars exacerbates existing alignment issues, necessitating intervention. In clinical practice, extraction of these third molars is a standard procedure to alleviate space constraints and restore ideal dental alignment. By removing wisdom teeth, dental practitioners aim to prevent further complications and preserve the integrity of the patient’s occlusion and overall oral health.

Impacted Wisdom Teeth and Their Complications
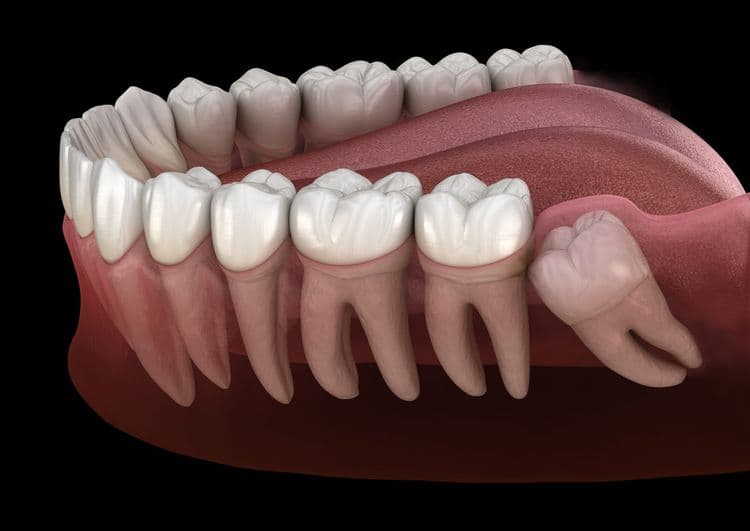
Impacted wisdom teeth, which fail to erupt properly due to insufficient space or misalignment, can lead to significant pain and discomfort. The obstruction of eruption pathways often results in pericoronitis, an infection characterized by inflammation and swelling of the surrounding gum tissue. Left untreated, these complications may progress to more severe infections or damage to adjacent teeth and bone structures, necessitating prompt surgical intervention.
Pain and Discomfort
When third molars become impacted, they often lead to significant pain and discomfort due to their inability to properly erupt through the gum tissue. This impaction can cause pressure against adjacent teeth and lead to periodontal complications. Clinicians evaluate the severity of discomfort using diagnostic imaging, such as panoramic radiographs, to assess the angulation and depth of impaction. Effective pain management is essential, typically involving analgesics and potential corticosteroids for inflammation reduction. Discomfort relief may also include localized anesthetics to numb the affected area. Surgical intervention is frequently recommended to alleviate persistent symptoms, involving an incision in the gingival tissue to remove the obstructed tooth. This procedure aims to restore oral function and prevent further complications related to impacted third molars.
Infection and Swelling
While third molars are known for their potential complications, the risk of infection and swelling is a primary concern in cases of impaction. Impacted wisdom teeth create an ideal environment for bacterial colonization due to partial eruption, leading to pericoronitis, a localized gum infection. The resultant inflammatory response often manifests as swelling, discomfort, and potential abscess formation. Infection prevention involves employing meticulous surgical techniques during extraction, ensuring thorough debridement and irrigation of the surgical site. Adherence to a rigorous post-operative care regimen, including prescribed antibiotics and antiseptic rinses, is vital in mitigating infection risk. Monitoring for signs of post-extraction complications, such as persistent edema or purulent discharge, is essential for timely intervention, ensuring ideal recovery and minimizing adverse outcomes.
The Risk of Infection and Inflammation
Infection and inflammation are significant concerns associated with retained wisdom teeth. Impacted or partially erupted wisdom teeth can create a breeding ground for bacteria, leading to pericoronitis—a localized infection. Effective infection prevention requires meticulous oral hygiene practices and potentially the use of antiseptic mouthwashes to minimize bacterial load. Inflammation management is essential, as chronic inflammation can precipitate periodontal disease or cyst formation. Clinicians often prescribe anti-inflammatory medications to alleviate symptoms. These complications necessitate thorough evaluation and timely intervention. Surgical extraction, when indicated, effectively eliminates the nidus of infection and inflammation. Additionally, postoperative care includes irrigation of the extraction site and adherence to prescribed antibiotic regimens to mitigate infection risks, ensuring a return to oral health and function.
Modern Diagnostic Techniques for Wisdom Teeth Assessment
In addressing the complications associated with wisdom teeth, a precise evaluation through modern diagnostic techniques becomes essential. Digital imaging, including panoramic radiographs, is crucial in visualizing the position and angulation of wisdom teeth relative to adjacent anatomical structures. These images provide significant insights into potential impactions or alignment issues. Complementing this, 3D scanning technology, such as cone-beam computed tomography (CBCT), offers volumetric data, enabling clinicians to assess the spatial relationships and proximity to critical structures like the mandibular nerve. This advanced imaging modality guarantees a thorough evaluation, aiding in determining the complexity of extraction procedures. Through these diagnostic advancements, dental professionals can formulate a strategic approach, minimizing intraoperative risks while enhancing patient outcomes related to wisdom teeth management.
Criteria for Deciding on Wisdom Teeth Extraction
Decisively determining the need for wisdom teeth extraction hinges upon a thorough evaluation of specific clinical criteria. Primary extraction criteria include impaction status, alignment, and potential for periodontal complications. A detailed dental evaluation involves radiographic imaging to identify impaction and angulation, determining whether teeth are partially erupted or fully submerged. Clinicians examine the anatomical proximity of wisdom teeth to adjacent structures, analyzing risks of damage to adjacent molars or the mandibular nerve. Presence of pathologies such as cysts or recurrent pericoronitis further influences the decision-making process. Additionally, overcrowding or malocclusion resulting from non-extracted wisdom teeth can necessitate removal. These evaluations guarantee that the decision to extract is grounded in minimizing potential complications and optimizing oral health outcomes.
Balancing Dental Health With Surgical Intervention
Evaluating the necessity for wisdom teeth extraction involves a careful balance between preserving dental health and the implications of surgical intervention. Preventive care emphasizes the importance of monitoring wisdom teeth for potential complications such as impaction, infection, or cyst formation. Dental professionals utilize radiographic imaging and clinical assessments to determine the likelihood of future dental issues. The decision to proceed with extraction considers surgical risks, including potential nerve damage, infection, and prolonged recovery. A thorough risk-benefit analysis guides clinicians in recommending the ideal course of action. In cases where the potential for disease outweighs surgical risks, extraction is often advised. Conversely, asymptomatic wisdom teeth with favorable positioning may warrant continued observation, minimizing unnecessary surgical exposure. This balanced approach guarantees patient-centric outcomes.
Frequently Asked Questions
What Are the Costs Involved in Wisdom Teeth Removal?
The costs involved in wisdom teeth removal vary, influenced by factors such as dental insurance coverage, procedure complexity, and anesthesia type. Payment plans may be available, assisting patients in managing financial obligations associated with this oral surgical procedure.
How Long Is the Recovery Time After Wisdom Teeth Extraction?
The recovery time post wisdom teeth extraction typically spans one to two weeks. Post operative care, including pain management and infection prevention, is essential for an efficient healing process, minimizing complications and ensuring ideal procedural outcomes.
Are There Alternative Treatments to Extraction for Problematic Wisdom Teeth?
In addressing problematic wisdom teeth, non-surgical options include preventive measures such as regular monitoring and dental hygiene optimization. Orthodontic interventions might realign teeth, while antibiotics can manage infections, offering temporary relief without extraction. Long-term efficacy varies.
Can Wisdom Teeth Removal Impact Jaw Alignment?
Wisdom teeth removal can affect jaw alignment due to potential changes in dental crowding and occlusion. Extraction procedures may alleviate crowding, possibly altering bite dynamics, but individual outcomes vary based on pre-existing dental conditions and anatomical structures.
What Are Common Side Effects Post Wisdom Teeth Extraction?
Common post-extraction side effects include localized swelling and discomfort. Pain management typically involves analgesics, while swelling reduction may benefit from cold compress application. Monitoring for complications, such as infection or dry socket, is essential for ideal recovery.