Root canal treatment becomes necessary when the pulp of a tooth becomes infected or inflamed. This condition often results from untreated cavities that allow bacteria to penetrate the enamel and dentin, reaching the pulp chamber. Additionally, dental trauma, including fractures or luxation, can expose the pulp or interrupt its blood supply, leading to necrosis. Repeated dental procedures also contribute to pulp damage. Understanding these causes is essential for preventing further complications and maintaining oral health.
Understanding Tooth Anatomy
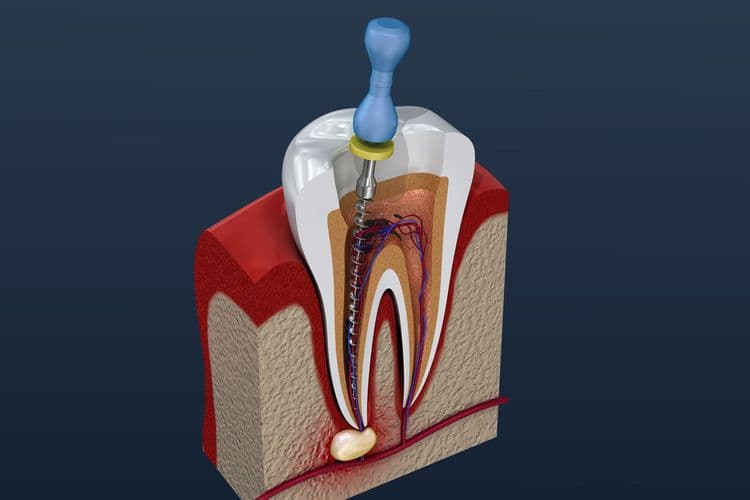
To fully comprehend the complexities of tooth structure, one must explore the intricate anatomy of the tooth. The dental structure is a sophisticated assembly consisting of several important layers. The outermost layer, enamel, is a highly mineralized tissue providing the primary defense against mechanical wear. Beneath this, the dentin comprises a dense, calcified tissue that supports the enamel and houses microscopic tubules. At the core lies the pulp chamber, rich in nerves and blood vessels, significant for tooth health. Tooth composition also includes cementum, a bone-like material covering the root, anchoring the tooth within the alveolar bone through the periodontal ligament. Understanding this detailed dental structure is important for diagnosing potential dental issues, including those that necessitate a root canal treatment.
The Role of Tooth Decay
Tooth decay initiates a cascade of events leading to the necessity for root canal treatment. Initially, demineralization compromises the tooth enamel, the outermost protective layer. This deterioration allows bacteria to infiltrate, forming cavities. As cavity progression advances, the structural integrity of the enamel is further compromised, enabling deeper penetration into the dentin, the softer, underlying tissue. This infiltration facilitates bacterial invasion into the pulp chamber, where nerves and blood vessels reside. Once bacteria reach this area, inflammation and infection can ensue, causing significant discomfort and potential abscess formation. If left untreated, the infection may spread, compromising the tooth’s viability. Therefore, prompt intervention is essential to arrest decay progression and prevent further complications, necessitating root canal therapy to salvage the tooth.
Impact of Dental Trauma
Dental trauma, a significant contributor to the need for root canal treatment, often arises from various forms of physical impact to the teeth. There exist multiple trauma types, including fractures, luxation, and avulsion, each inducing distinct injury effects on dental structures. Fractures can compromise enamel and dentin, potentially exposing the pulp and leading to irreversible pulpitis. Luxation injuries, characterized by the displacement of teeth, can sever neurovascular supply, resulting in pulpal necrosis. Avulsion, the complete dislodgement of a tooth, poses a risk of pulp damage if reimplantation is delayed. These trauma types disrupt the integrity of the pulp, necessitating endodontic intervention to preserve or restore dental function. Understanding these injury effects is vital for appropriate clinical management and prevention of further complications.
Repeated Dental Work
Repeated dental procedures can progressively compromise the structural integrity of a tooth, rendering it susceptible to damage. Each intervention, including fillings, crowns, or adjustments, may incrementally weaken the tooth’s natural defenses. Consequently, this structural weakening can facilitate bacterial penetration, heightening the risk of infection and potentially necessitating root canal therapy.
Tooth Structure Weakening
When a tooth undergoes multiple dental procedures, its structural integrity can become compromised, leading to an increased risk of requiring a root canal. Repeated interventions, such as fillings, crowns, or veneers, contribute to tooth erosion and enamel loss. The cumulative effects of these procedures weaken the tooth’s natural defenses. Enamel, the tooth’s hardest outer layer, provides protection against mechanical forces and bacterial invasion. However, each dental treatment involves some degree of enamel removal or alteration, which diminishes its protective capacity. As enamel erodes, the underlying dentin becomes exposed, reducing the tooth’s ability to withstand stress and pressure. This weakening of the tooth’s structure can result in cracks or fractures, potentially necessitating root canal therapy to address compromised dental health.
Increased Infection Risk
As dental work is performed repeatedly on a tooth, the potential for infection increases considerably due to the cumulative disruption of the tooth’s natural barriers. Each intervention, such as fillings, crowns, or adjustments, may compromise the tooth’s integrity, creating microscopic openings. These allow increased bacteria to penetrate deeper into the dentin and pulp chambers. The resultant bacterial colonization can overwhelm the tooth’s immune defenses, leading to infection. Poor oral hygiene exacerbates this risk by failing to remove bacterial biofilms that thrive in these compromised areas. The progressive invasion of bacteria can necessitate a root canal to eliminate infection and preserve the tooth structure. Hence, meticulous oral hygiene and minimizing repeated dental procedures are critical in reducing infection incidences.
Cracks and Chips in Teeth
Cracks and chips in teeth, whether due to trauma, bruxism, or age-related wear, can compromise the integrity of dental structures and increase the risk of needing a root canal. Tooth fractures may expose the dental pulp, which contains nerves and blood vessels, making it susceptible to bacterial invasion. This exposure can lead to pulpitis, an inflammation that often necessitates endodontic intervention. Chips may initially seem minor but can progressively worsen, potentially leading to significant structural damage. Dental restoration is essential for repairing these fractures and chips, as it involves materials and techniques that restore the tooth’s function and aesthetics. However, if the pulp becomes irreversibly damaged despite restoration efforts, a root canal may be the only viable solution to preserve the tooth.

Gum Disease and Its Consequences
Although often overshadowed by more immediate dental issues, gum disease plays a critical role in the potential need for a root canal. Gum inflammation, a hallmark of periodontal disease, contributes to the development of periodontal pockets. These pockets form when the gums pull away from the teeth, creating spaces where bacteria can accumulate. Over time, this accumulation leads to the destruction of the supporting bone and ligament structures surrounding the teeth. As periodontal pockets deepen, they provide a pathway for bacteria to infiltrate the tooth’s root system. This infiltration can result in infection of the dental pulp, necessitating endodontic intervention. Consequently, managing gum health is essential to prevent progression to conditions requiring root canal treatment, maintaining both periodontal and endodontic health.
Signs and Symptoms of Pulp Infection
The clinical presentation of pulp infection is characterized by distinct signs and symptoms including localized pain and heightened sensitivity to thermal stimuli. Patients may also exhibit gingival swelling, tooth discoloration, and persistent halitosis, indicative of necrotic tissue within the pulp chamber. These manifestations warrant prompt diagnostic evaluation to prevent progression to irreversible damage necessitating endodontic intervention.
Pain and Sensitivity
Why does the experience of pain and sensitivity often signal a pulp infection within a tooth? When the dental pulp becomes inflamed due to bacterial invasion or trauma, it triggers nociceptors, which are pain receptors. This inflammation results in heightened sensitivity to thermal stimuli and pressure, indicating a compromised pulp. Clinicians recognize this as a key diagnostic indicator of pulp pathology. Managing this discomfort involves both pain management and sensitivity reduction strategies. Pain management may include analgesics to alleviate discomfort, while sensitivity reduction focuses on desensitizing agents to mitigate exaggerated responses to stimuli. These interventions aim to stabilize the condition and prevent progression to more severe stages, such as abscess formation, thereby potentially avoiding the necessity for root canal therapy.
Swelling and Discoloration
When a pulp infection progresses, it frequently manifests as swelling and discoloration of the affected tooth and surrounding tissues. Swelling results from tissue inflammation, a response to bacterial proliferation within the dental pulp chamber. This inflammation can extend to the periodontal ligament and adjacent gingival tissues, exacerbating discomfort. Discoloration is indicative of necrotic pulp tissue, often presenting as a greyish or darkened hue of the tooth. This color change signals the breakdown of hemoglobin within the pulp due to root infection. Clinically, these symptoms suggest compromised vascular supply and increased intrapulpal pressure, necessitating prompt intervention. Diagnostic evaluation commonly includes radiographic imaging to assess the extent of infection and tissue involvement, guiding appropriate endodontic treatment to alleviate symptoms and restore dental health.
Persistent Bad Breath
Beyond swelling and discoloration, persistent bad breath, or halitosis, emerges as a significant indicator of pulp infection. This condition arises when bacterial activity within the necrotic pulp tissue produces volatile sulfur compounds (VSCs), leading to persistent halitosis. The compromised dental pulp creates an environment conducive to anaerobic bacterial proliferation. These bacteria metabolize proteins, releasing malodorous byproducts. Such halitosis is not alleviated by conventional dental hygiene practices, as the source is internal rather than superficial. Persistent halitosis, consequently, necessitates a thorough clinical assessment to ascertain its etiology. If pulp infection is confirmed, a root canal procedure may be warranted to eradicate the infection and restore oral health. Effective management of pulp infection is vital to preventing further dental complications.
How Bacteria Reach the Tooth Pulp
Bacteria reach the tooth pulp primarily through the progression of dental caries, which compromise the integrity of the enamel and dentin. Initially, demineralization occurs as acids produced by oral bacteria dissolve the hard surfaces of the tooth, facilitating bacterial invasion. As caries advance, they breach the enamel, allowing bacteria to infiltrate the underlying dentin. This invasion progresses toward the pulp chamber, where the soft tissue resides. Pulp exposure becomes imminent when bacterial activity breaks down the dentin, creating pathways for microorganisms to invade the pulp. Once the pulp is exposed, an inflammatory response is triggered, potentially leading to pulpitis or necrosis. The breach of protective barriers results in increased vulnerability, escalating the risk of infection and necessitating endodontic intervention.
The Importance of Timely Dental Care
Prompt dental intervention plays a critical role in preserving oral health and preventing the escalation of dental issues. Timely care, incorporating preventive measures and regular checkups, is essential in identifying potential problems before they necessitate invasive procedures like root canals. Regular dental examinations allow for the early detection of caries or periodontal diseases, which can compromise tooth structure and lead to pulp exposure. By adhering to a schedule of regular checkups, patients greatly reduce the risk of bacterial infection reaching the tooth pulp. Preventive measures, such as professional cleanings and fluoride treatments, further mitigate the progression of decay. To summarize, consistent dental oversight is indispensable in maintaining oral health, averting the need for more complex treatments, and ensuring long-term dental well-being.
Frequently Asked Questions
Can Poor Oral Hygiene Lead to a Root Canal?
Yes, poor oral hygiene can lead to a root canal. Oral bacteria accumulate, forming dental plaque. This plaque can cause tooth decay, eventually reaching the pulp and necessitating a root canal to remove the infected tissue.
How Does Diet Influence the Need for a Root Canal?
Excessive sugar intake and frequent consumption of acidic foods can demineralize tooth enamel, leading to cavities. These cavities, if untreated, may progress to pulp infection, increasing the likelihood of requiring a root canal procedure.
Are Certain Medications Linked to Increased Root Canal Risk?
Certain medications, due to their side effects, may impact dental health by reducing saliva production, which can lead to increased plaque buildup and decay. This indirect effect might elevate the risk of needing a root canal treatment.
Does Genetics Play a Role in Root Canal Susceptibility?
Genetic predisposition and hereditary factors may influence an individual’s susceptibility to root canal treatment. These factors can impact dental development, enamel strength, and immune response, potentially increasing the risk of conditions necessitating endodontic intervention.
What Lifestyle Habits Increase the Likelihood of Needing a Root Canal?
Lifestyle habits such as smoking and teeth grinding greatly increase the likelihood of needing a root canal. Smoking effects include reduced blood flow, while teeth grinding causes enamel wear, both leading to increased vulnerability to dental infections or damage.