Dental health often hinges on the nuanced distinction between root canals and cavities, two common but fundamentally different procedures. Cavities typically affect the enamel and dentin, requiring fillings to restore structural integrity. However, when decay penetrates deeper, reaching the pulp, a root canal becomes imperative to remove infected tissue. Each procedure varies in complexity, recovery, and impact on daily life, prompting a closer examination of their respective processes and implications.
Understanding Dental Anatomy
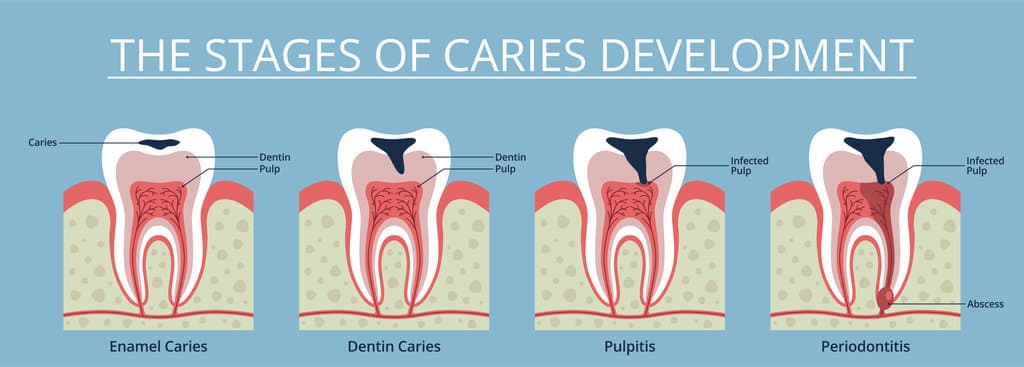
Dental anatomy forms the foundational framework for understanding the distinction between a root canal and a cavity. Tooth anatomy consists of multiple layers: enamel, dentin, pulp, and cementum, each serving specific functions within the dental structure. The enamel, being the outermost layer, provides a hard protective shell, while dentin lies beneath, acting as a secondary barrier. The pulp, residing centrally, contains nerves and blood vessels essential for tooth health. Cementum, covering the tooth’s root, anchors it within the periodontal ligament. Understanding these components is imperative to differentiate between dental issues. A cavity, or carious lesion, typically affects the enamel and dentin, whereas a root canal procedure involves the pulp chamber, addressing infections or damage to the pulp tissue.
What Causes Cavities?
Cavities are primarily caused by the consumption of sugary foods and drinks, which contribute to the proliferation of bacterial plaque on the teeth. Poor oral hygiene practices exacerbate this condition by allowing the plaque to persist and metabolize sugars into acids, leading to demineralization of the enamel. Evidence indicates that without regular removal of plaque through brushing and flossing, the risk of cavity development greatly increases.
Sugary Foods and Drinks
While the consumption of sugary foods and drinks may seem innocuous, it plays a pivotal role in the development of dental cavities. When sugar consumption occurs, oral bacteria metabolize the sugars, producing acids as byproducts. These acids contribute to dental erosion by demineralizing the enamel, the tooth’s protective outer layer. Repeated exposure to such acids can compromise enamel integrity, leading to the formation of cavities. Scientific studies have demonstrated a direct correlation between high sugar intake and increased incidence of carious lesions. Importantly, the frequency of sugar exposure is more detrimental than quantity, as prolonged acid production exacerbates enamel erosion. Consequently, reducing sugar consumption can mitigate the risk of cavity formation, underscoring the importance of dietary modifications in dental health maintenance.
Poor Oral Hygiene
Inadequate oral hygiene routines greatly contribute to the development of dental cavities, as insufficient cleaning allows plaque—a sticky film of bacteria—to accumulate on the teeth. Poor hygiene practices, such as irregular brushing and flossing, fail to remove food particles and debris, which serve as a substrate for bacterial growth. Dental neglect exacerbates this condition, leading to the demineralization of tooth enamel. Over time, the acids produced by bacterial metabolism erode the enamel, creating cavities. Evidence suggests that individuals who brush less than twice a day or neglect regular dental check-ups are at a higher risk of cavity formation. Furthermore, the absence of fluoride-containing toothpaste in daily oral care routines further diminishes enamel resilience, making teeth more susceptible to decay.
Bacterial Plaque Formation
Bacterial plaque, a biofilm that adheres to the tooth surface, is a primary etiological factor in the formation of dental cavities. This biofilm comprises a diverse microbial community where bacterial growth is facilitated by dietary sugars and poor oral hygiene. Streptococcus mutans and other acidogenic bacteria metabolize sugars, producing acids that demineralize the tooth enamel. This demineralization process leads to cavity formation over time if left unchecked. Effective plaque removal is vital in disrupting the bacterial colonization process and preventing acid production. Regular mechanical disruption, such as brushing and flossing, aids in the physical removal of plaque. Additionally, chemical agents like fluoride enhance remineralization and reduce bacterial adhesion. Maintaining ideal oral hygiene practices is essential to mitigate cavity risk effectively.
Signs and Symptoms of Cavities
Detecting cavities early is essential for effective management and prevention of further dental complications. Early indicators include tooth sensitivity to thermal stimuli and sweet substances, often signifying enamel compromise. Visual signs such as discoloration issues, including white spots or brownish lesions, may appear as the demineralization process progresses. Persistent pain and swelling areas can indicate pulp involvement or infection. Bad breath, associated with bacterial accumulation, is another symptom. Food traps, where particles get lodged in pits or grooves, exacerbate decay risk. These manifestations result from acidogenic bacteria metabolizing fermentable carbohydrates, leading to enamel demineralization. Prompt identification of these symptoms through clinical examination aids in mitigating the progression of carious lesions and averts the necessity for more invasive procedures.
The Cavity Treatment Process
Addressing cavities involves a systematic treatment process designed to restore tooth integrity and function while preventing further decay. Initially, cavity detection is paramount, utilizing diagnostic tools such as radiographs and visual examination to identify carious lesions. Once diagnosed, the dentist removes the decayed tissue using precision instruments, ensuring all compromised enamel and dentin are excised. This step is vital to halt the progression of decay. Following cavity preparation, the void is filled using dental fillings. These restorative materials, which can include amalgam, composite resins, or glass ionomer cements, are selected based on the cavity’s location, size, and patient-specific factors. The filling process restores the tooth’s structural integrity, ensuring functional longevity while providing an effective barrier against bacterial invasion.
When a Root Canal Becomes Necessary
While cavity treatment focuses on removing decayed material and filling the resultant void, there are instances where the decay penetrates deeper, affecting the tooth’s pulp, thereby necessitating a root canal procedure. Root canal necessity arises when bacterial invasion leads to pulpitis, an inflammation of the dental pulp. This condition can result from extensive decay, trauma, or multiple dental procedures. In such cases, the compromised pulp may cause severe pain or abscess formation, escalating to dental emergency situations if untreated. The root canal procedure involves the meticulous removal of infected pulp, followed by disinfection and sealing of the root canals. This intervention not only alleviates pain but also preserves the tooth structure, preventing further complications. Evidence supports root canal treatment as an effective solution for pulpitis-induced emergencies.
Signs and Symptoms of Root Canal Issues
How can one identify the onset of root canal problems? Initial indications often include tooth sensitivity to thermal stimuli or sweet substances. Persistent pain, especially when not directly stimulated, can signify underlying pulp tissue damage. Swelling gums around the affected tooth may suggest inflammatory processes or infection. Discoloration issues, such as a darkened tooth, can indicate necrotic pulp tissue. Additionally, the presence of a dental abscess, characterized by pus-filled pockets, may result from bacterial infiltration and further corroborate the need for endodontic intervention. Biting discomfort is another critical symptom, signaling compromised structural integrity or heightened pressure sensitivity within the tooth. These clinical manifestations, when evaluated collectively, provide substantial evidence of potential root canal pathology requiring professional assessment and intervention.
The Root Canal Procedure Explained
The root canal procedure is a multi-step treatment that begins with the administration of local anesthesia to guarantee patient comfort, followed by the removal of infected pulp tissue from the tooth’s interior. Pain management techniques are critically integrated throughout the process, utilizing both pharmacological agents and advanced technology to minimize discomfort. Post-procedure, patients are provided with detailed recovery and aftercare instructions, emphasizing the importance of oral hygiene and follow-up appointments to guarantee successful healing and restoration of dental function.
Steps Involved in Procedure
When a tooth becomes severely decayed or infected, a root canal procedure may be necessary to restore its function and health. The procedure begins with patient preparation, where the dentist conducts a thorough examination and takes radiographic images to assess the extent of infection. A local anesthetic is administered to guarantee the patient’s comfort. The procedure overview involves isolating the tooth with a dental dam to maintain a sterile environment. An access opening is created in the crown of the tooth, allowing the dentist to remove infected pulp tissue using specialized instruments. The canals are meticulously cleaned, shaped, and disinfected. The final step involves sealing the canals with a biocompatible material and restoring the tooth with a filling or crown to guarantee structural integrity.
Pain Management Techniques
Although the notion of undergoing a root canal procedure may evoke anxiety due to anticipated discomfort, advancements in pain management techniques have significantly minimized patient distress. Local anesthesia is the cornerstone, effectively numbing the targeted dental area. This is often supplemented by over the counter medications such as ibuprofen or acetaminophen to manage postoperative pain and inflammation. Additionally, relaxation techniques play an essential role in alleviating patient anxiety, contributing to an overall reduction in perceived pain levels. Techniques such as deep breathing exercises and guided imagery are often recommended to help patients remain calm during the procedure. Dentists may also employ sedation methods, including nitrous oxide or oral sedatives, to enhance patient comfort throughout the treatment process.
Recovery and Aftercare Tips
Many patients find that understanding the recovery process and following precise aftercare instructions can greatly enhance the healing experience following a root canal procedure. Post treatment care is vital in preventing complications such as infection or inflammation. Patients are typically advised to avoid chewing on the treated tooth until full restoration is completed, minimizing pressure on the temporary filling. Dietary restrictions play an important role; soft foods are recommended to prevent damage to the treated area. Additionally, maintaining ideal oral hygiene, including gentle brushing and flossing, is essential to reduce bacterial proliferation. Over-the-counter analgesics may be recommended to manage mild discomfort. Follow-up appointments are necessary to monitor healing progress and confirm the tooth’s structural integrity is restored effectively.
Comparing Recovery and Aftercare
In the domain of dental procedures, recovery and aftercare present distinct pathways for root canal therapy and cavity fillings, each characterized by specific protocols and expectations. Post-root canal therapy, individuals often experience moderate pain levels that typically subside within a few days, as inflammation decreases. The healing timeline is generally extended, with complete tissue recovery taking weeks. In contrast, cavity fillings involve minimal discomfort, with pain levels usually limited to mild sensitivity, and a rapid healing timeline, often allowing patients to resume normal activities within hours. Aftercare for root canals necessitates diligent oral hygiene and follow-up visits to guarantee restoration stability. Conversely, cavity fillings require less intensive aftercare, mainly focusing on maintaining dental hygiene to prevent recurrence of decay.
Preventive Measures for Dental Health
Ensuring ideal dental health involves a thorough approach to preventive measures, strategically designed to mitigate the onset of cavities and the necessity for more invasive treatments like root canals. Regular dental check ups play a critical role, allowing for the early detection of dental caries and other oral pathologies. These routine examinations provide opportunities for professional cleaning, plaque removal, and the reinforcement of dental hygiene practices. Evidence suggests that optimal dental hygiene, including proper brushing and flossing techniques, greatly reduces the accumulation of bacterial biofilm, a key etiological factor in cavity formation. Additionally, the use of fluoride and dental sealants is proven to enhance enamel resistance. These preventive strategies collectively function to sustain oral health, minimizing the need for restorative procedures such as root canals.
Frequently Asked Questions
Can a Root Canal Be Avoided if a Cavity Is Detected Early?
Early cavity detection is essential for root canal prevention. If cavities are identified at an initial stage, less invasive treatments can be employed, reducing the risk of pulp infection, thereby potentially eliminating the need for a root canal procedure.
How Long Does a Root Canal Procedure Typically Take?
The typical procedure duration for a root canal ranges from 60 to 90 minutes, contingent on tooth complexity. Patient experience involves localized anesthesia application, pulp removal, cleaning, and sealing, ensuring minimal discomfort and restoring tooth functionality effectively.
Are There Alternative Treatments to a Root Canal for Severe Cavities?
For severe cavities, alternatives include tooth extraction or exploring natural remedies. However, natural remedies lack scientific backing for reversing decay. Tooth extraction is a definitive solution but results in permanent tooth loss, necessitating prosthetics for function restoration.
What Are the Cost Differences Between a Cavity Filling and a Root Canal?
The cost comparison reveals that cavity fillings generally incur lower expenses than root canals. Insurance coverage often influences out-of-pocket costs, with root canals typically requiring higher patient contributions due to their complexity and extended procedural requirements.
How Can I Tell if I Need a Root Canal Rather Than a Filling?
To assess the need for a root canal versus a filling, symptom identification is essential. Examine pain intensity, duration, and sensitivity to temperature changes. Detailed pain assessment aids in determining if pulp infection necessitates a root canal.


